Stress Urinary Incontinence
What is stress urinary incontinence?
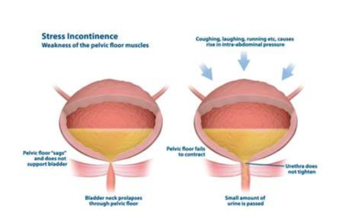
Stress urinary leakage is the involuntary loss of urine because of an increase in abdominal pressure. This typically occurs with activities such as coughing, sneezing, straining, lifting or running. It is caused by the muscles of the pelvic floor not being strong enough to stop urine leaking out, when the bladder is under pressure.
What causes stress incontinence?
In women
-
pregnancy,
-
childbirth via the vagina,
-
vaginal hysterectomy
-
being postmenopausal
all increase the risk of stress incontinence.
Pregnancy and childbirth affect the pelvic floor muscles and tendons causing them to either weaken or tear. If you have 2 or fewer pregnancies then caesarean sections reduce the risk of subsequent stress incontinence. If you have had 3 or more pregnancies then the risk of subsequent stress incontinence does not seem to be changed by how the baby is delivered. The more children you have unfortunately the more likely you are to have stress urinary incontinence.
In men stress leakage of urine can occur after surgery on the prostate such as a radical prostatectomy or a rebore of the prostate (TURP). This is due to damage to the urinary sphincter during surgery.
For an animated explanation of stress incontinence see:
https://www.youtube.com/watch?v=3KRhhxVfGH0https
What test might be needed?
You should have a urine test done (MSU) to check for blood in the urine or infections, sometimes a flow test and bladder scan and if conservative therapy has failed undergo a special test called urodynamics.
How should my stress incontinence be treated?
The best initial treatment is pelvic floor physiotherapy. This strengthens the pelvic floor and reduces leakage of urine. If this fails then surgical options can be explored. Before surgery is offered you will need to have a test called urodynamics. If your leakage has occurred after surgery then often time itself allows the leakage to stop as the body heals. So in summary we can use
-
pads
-
pelvic floor exercises
-
surgery.
What are incontinence pads?
It is really important to use the correct product or pad. Pads for urine leakage are designed to wick away the water, so you stay dry, are more absorbent and so work much better. Pads for menstrual loss are not good at dealing with urine, which is really just water. Often people are embarrassed to use incontinence pads or buy them and use menstrual pads instead, but that is not a good idea as the amount of water a menstrual pad can hold is quite small.
For men there are triangle shaped pads to surround the penis. The standard one is made by Tena. There come in different absorbancies. The lightest is called level 1. There is a sticky strip which attaches the pad to your underpants so the pad doesn’t move around.
Pads for women are much longer and more narrow. The amount of urine a pad can hold is shown by the number of raindrops on the side of the packet. For women this can be form ½ a drop to 4 drops.
What are the pelvic floor muscles?
The pelvic muscles pass form a sling or hammock which pass from the front pelvic bone (the symphysis pubis) to the bottom of the spine (the sacrum). They also pass from one side of the pelvis to the other. If you looked down on them from above they look a little like two hands cupped together. Through the pelvic floor pass the tube you pee through (urethra), the rectum and in women the vagina. These openings create potential weaknesses in the pelvic floor.
What is pelvic floor physiotherapy?
Pelvic floor physiotherapy is a series of exercises to increase the strength of the pelvic floor muscles. This is often called Kegel exercises after the doctor who first popularised them. As they are often done poorly, it can be very helpful to see a physiotherapist who specialises in this area. As we can see above the pelvic floor muscles attach to the pelvis and the pelvis in turn attaches to the spine. It is therefore important to also work on your core muscle strength. If your core is strong then the pelvis is stabilised and the exercises work better.
If the exercises do not work then you may need surgery. Before having surgery you should have a test called urodynamics.
What is urodynamics?
Urodynamics is a test designed to see how the bladder is working and why it is leaking urine . It helps us decide what operation or medication can be used to treat the incontinence. In Hamilton the usual form of urodynamics is called video-urodynamics. Video-urodynamics are carried out in the x-ray department. A catheter is placed in the bladder and one in your rectum. The bladder is filled slowly and pressure readings are taken from the bladder and rectum. Once the bladder is full you will be asked to cough and then to pee to measure how hard the bladder works during peeing.
During the study x-rays are taken to look at the shape of the bladder and the bladder neck. During coughing we look to see if the bladder neck descends or stays in place and if leakage can be stopped by a pelvic floor contraction.
What operations are available if physiotherapy has not worked?
The surgical options are different for men and women. For women a support can be placed behind the urethra. This support can be made out of mesh or out of a piece of tissue for your body (pubovaginal sling). This is discussed more fully in the section SURGERY FOR FEMALE STRESS URINARY INCONTINENCE. In men the operations are either y to lift the urethra up, compress the urethra or to put a valve (cuff) around the tube you pee through. Please see TREATMENT OF URINARY INCONTINENCE IN MEN.
Youtube videos on pelvic floor physiotherapy
For men:
https://www.youtube.com/watch?v=dSqK4_3YSMI
https://www.youtube.com/watch?v=QHwVglPQR_w
https://www.youtube.com/watch?v=5IbliBiRzOw
pilates exercises
https://www.youtube.com/watch?v=1CNBL597hxA
https://www.youtube.com/watch?v=gidN1N8nSRU
For women:
https://www.pelvicexercises.com.au
https://www.youtube.com/watch?v=c9UDKATwuVA&list=PL2N-dN9DIUrSnPERQ-MNN-tLX4gsFyVQZ&index=3
Very comprehensive medical reviews:
http://uroweb.org/wp-content/uploads/20-Urinary-Incontinence_LR.pdf
https://www.auanet.org/education/guidelines/incontinence.cfm